5 Tips for Senior Living Emergency Preparedness
Natural disasters, power outages, medical emergencies, and other unexpected events can strike at any time. For assisted living facilities, having a robust emergency preparedness plan isn’t just recommended, it’s essential for protecting the vulnerable residents in your care.
Over the past two decades working with assisted living facilities across California, the Assisted Living Education staff has witnessed firsthand how proper emergency preparedness can mean the difference between chaos and calm during a crisis.
From the devastating wildfires that swept through Northern California to the widespread power outages that left communities in darkness, facilities with comprehensive emergency plans were able to continue providing quality care while others struggled to maintain basic operations.
Understanding Emergency Preparedness in Assisted Living
Emergency preparedness in assisted living environments requires a unique approach compared to other residential settings. The residents you serve often have mobility limitations, cognitive impairments, or medical conditions that make evacuation and emergency response more complex.
Around 75% of RCFEs felt well prepared for fires and infectious disease outbreaks, had mixed preparedness levels for earthquakes and floods, and felt least prepared for landslides and active shooter emergencies.
For those wondering what is a RCFE, these facilities serve adults aged 60 and older who need assistance with daily activities but don’t require intensive nursing care. This population requires specialized emergency planning that considers their unique vulnerabilities and care needs.
Tip 1: Develop a Comprehensive Risk Assessment and Hazard Analysis
The foundation of effective emergency preparedness begins with understanding the specific threats your facility faces. Every assisted living home should conduct a thorough hazard vulnerability analysis (HVA) that examines both natural and human-made risks in your geographic area.
Start by identifying the most likely emergencies your facility could face. In California, this typically includes earthquakes, wildfires, flooding, and power outages. However, don’t overlook less obvious threats such as infectious disease outbreaks, chemical spills from nearby facilities, or even active shooter situations.
Consider the case of Sunset Manor, a 45-bed RCFE in Sonoma County. They had a basic fire evacuation plan but hadn’t considered the unique challenges posed by wildfire smoke. After conducting a comprehensive HVA, they realized that air quality issues could force them to shelter-in-place for extended periods, requiring additional air filtration systems and modified activity schedules.
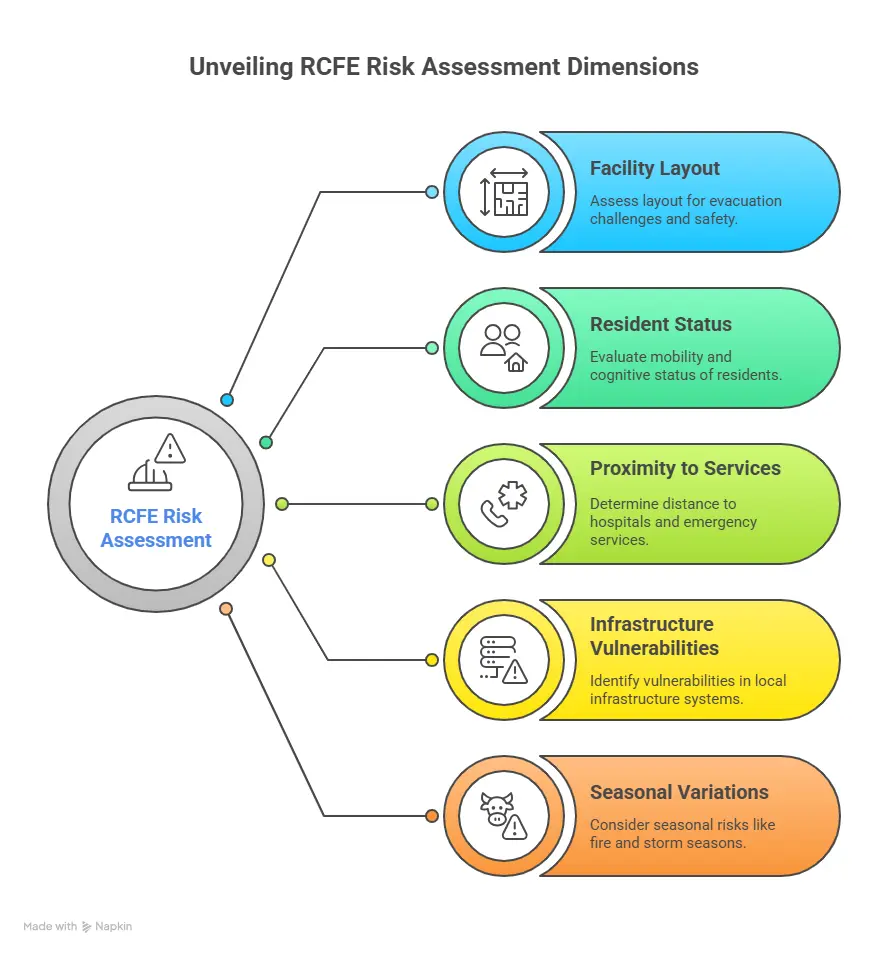
Your risk assessment should evaluate not just the likelihood of each emergency, but also the potential impact on your specific resident population.
Consider factors such as:
- The physical layout of your facility and potential evacuation challenges
- The mobility and cognitive status of your residents
- Your facility’s proximity to hospitals and emergency services
- Local infrastructure vulnerabilities (power grids, water systems, communication networks)
- Seasonal variations in risk (fire season, storm season, etc.)
Tip 2: Create Detailed Communication Plans and Protocols
During emergencies, clear communication can literally save lives. Your facility needs multiple communication strategies that work even when primary systems fail. This includes maintaining contact with residents’ families, coordinating with emergency services, and ensuring staff can communicate effectively with each other.
Develop a communication tree that includes primary and backup contact methods for all stakeholders. This should encompass resident emergency contacts, staff members, local emergency services, healthcare providers, and regulatory agencies. Remember that phone lines may be down during major emergencies, so consider alternative communication methods such as text messaging, social media, or two-way radios.
Many disaster preparation tips for an RCFE facility emphasize the importance of redundant communication systems. Consider investing in battery-powered or hand-crank radios, satellite phones for extreme situations, and establishing communication protocols with neighboring facilities for mutual aid.
Your communication plan should also address how you’ll keep residents and families informed during extended emergencies. Regular updates help reduce anxiety and demonstrate that you’re maintaining control of the situation. Designate specific staff members to handle external communications so that your administrative team can focus on resident care.
Tip 3: Implement Comprehensive Staff Training and Regular Drills
Even the most detailed emergency plan is worthless if your staff doesn’t know how to execute it effectively. Regular training and practice drills are crucial for ensuring everyone knows their role during an emergency.
Your training program should cover all types of emergencies your facility might face, not just fire evacuation. Staff should understand evacuation procedures, shelter-in-place protocols, medical emergency response, and how to assist residents with various mobility and cognitive limitations.
Consider the complexity of a day in the life of an RCFE administrator and how emergency situations add additional layers of responsibility. Your training should prepare staff to handle these increased demands while maintaining quality care for residents.
Practice drills should be conducted at different times and under varying conditions to ensure staff can respond effectively regardless of when an emergency occurs. DSS requires a fire drill every three months and disaster drills every six months.
Include scenarios where key staff members are unavailable, forcing others to step into leadership roles. This cross-training approach ensures continuity of operations even when your primary emergency response team isn’t available.
Document all training activities and maintain records of staff competencies. This documentation demonstrates compliance with regulatory requirements and helps identify areas where additional training may be needed. Many California RCFE administrator certification training programs now include enhanced emergency preparedness training, reflecting the growing recognition of its importance.

Prepare both your staff and the senior residents with ongoing talks and drills about emergency preparedness.
Tip 4: Maintain Adequate Emergency Supplies and Equipment
During emergencies, your facility may need to operate independently for 72 hours or longer before outside assistance arrives. This requires maintaining emergency supplies that can sustain both residents and staff during extended disruptions.
Your emergency supply inventory should include:
- Food and water for at least 72 hours (one gallon of water per person per day)
- Medications and medical supplies
- Battery-powered lighting and radios
- First aid supplies and emergency medical equipment
- Backup power sources (generators, battery systems)
- Personal protective equipment
- Sanitation and hygiene supplies
- Blankets and emergency clothing
- Tools and equipment for facility maintenance
Don’t forget about the special needs of your resident population. Many assisted living residents require specialized equipment such as wheelchairs, walkers, or medical devices. Ensure you have backup equipment and batteries for electronic devices that residents depend on. Also, residents on special diets, such as puree diets, will require special considerations if there is no power.
Regularly inspect and rotate your emergency supplies to ensure they remain usable when needed. Establish relationships with local suppliers who can provide emergency restocking if needed. Consider joining mutual aid agreements with other facilities in your area to share resources during large-scale emergencies.
Tip 5: Establish Clear Evacuation Procedures and Shelter-in-Place Protocols
Not every emergency requires evacuation, and in some cases, sheltering in place may be the safest option for your residents. Your facility needs detailed procedures for both scenarios, with clear decision-making criteria for determining which approach to take.
Your evacuation plan should address the unique challenges of moving elderly residents, some of whom may have mobility limitations or cognitive impairments. This includes having adequate transportation arranged in advance, knowing which residents require special assistance, and maintaining portable resident records that can accompany evacuees.
Consider partnering with local transportation companies or other care facilities to ensure you have access to appropriate vehicles and temporary housing if needed.
Your senior living emergency disaster plan should include detailed evacuation routes, assembly points, and procedures for accounting for all residents and staff.
Shelter-in-place procedures are equally important, particularly for emergencies involving hazardous materials, severe weather, or security threats. These protocols should address how to seal the facility from outside contaminants, maintain life support systems, and keep residents comfortable during extended periods of confinement.
The Regulatory Landscape and RCFE Requirements
California has significantly strengthened emergency preparedness requirements for assisted living facilities in recent years. These enhanced RCFE requirements reflect lessons learned from recent disasters and the growing recognition that emergency preparedness is a fundamental aspect of resident safety.
CDSS just released a new Provider Information Notice (PIN) – 25-10-CCLD – to address preparations for extreme heat, wild fires, public safety power shutoffs and West Nile virus.
Facilities must now update their emergency preparedness plans with additional specificity, enhance staff training programs, and conduct regular drill exercises. The regulations also require facilities to purchase evacuation chairs and other specialized equipment to assist residents with mobility challenges.
For administrators working toward their California RCFE administrator certification, understanding these requirements is essential. The certification process now includes comprehensive coverage of emergency preparedness topics, reflecting the critical importance of these skills in modern assisted living administration.
Looking Forward: Building Resilience in Your Facility
Emergency preparedness isn’t a one-time project, it’s an ongoing process that requires regular review and updates. As your resident population changes, as new threats emerge, and as you learn from each emergency drill or real-world event, your plans should evolve accordingly.
Consider appointing an emergency preparedness coordinator who can focus specifically on maintaining and improving your facility’s readiness. This person should stay current on best practices, regulatory changes, and lessons learned from emergencies in other facilities.
Building a culture of preparedness among your staff and residents also contributes to overall resilience. When everyone understands the importance of emergency preparedness and their role in the process, your facility becomes better equipped to handle whatever challenges may arise.
Remember that emergency preparedness is ultimately about protecting the people you serve. The residents in your care have chosen to trust you with their safety and well-being. By implementing comprehensive emergency preparedness measures, you’re honoring that trust and ensuring that you can continue providing excellent care even in the most challenging circumstances.
The investment in emergency preparedness pays dividends not just during actual emergencies, but in the daily confidence it provides to residents, families, and staff.
When everyone knows that thorough preparations are in place, it creates an environment where people can focus on what matters most; living well and providing quality care.
In addition, Assisted Living Education’s Emergency Disaster Plan manual provides the reference material and updated COVID-19 preparedness required by DSS.